Gen Med Station 5
Station 5
A really bad cough!
Candidate Instructions
Setting:
You are a junior doctor working in A+E. This patient has presented with a cough.
Name: Tony Rogers
Tasks:
1. Take a history from the patient.
2. Interpret the provided investigations.
3. State your differential diagnosis to the examiner.
4. Explain your management to the examiner.
Simulated Patient Instructions
Briefing
Diagnosis: Atypical pneumonia presenting as a cough and fever.You are Tony Rogers (Age: 41)
You have presented to the Emergency Department with a cough.
Appearance and Behaviour
You should aim to look visibly nervous, especially when talking about the fact you've already had one set of antibiotics that didn't work..
Opening statement
“I have this cough that won’t go away and recently I’ve been feeling absolutely terrible”
Information to Give Freely
You noticed that you had started coughing about 2 weeks ago. You did a COVID PCR that came back negative. The GP started you on antibiotics but they haven’t worked, the cough has just been getting worse.
Presenting Complaint
Symptom - coughOnset - 2 weeks ago
Character – You’ve been bringing up green sputum, the amount has increased despite the antibiotics. Only if asked - you haven’t brought up any blood.
Associated symptoms - you’ve been feverish (highest you measured was 39C) and breathless (even if you aren’t doing anything) over the last few days. You almost fainted today which is why your wife asked you to come in. If asked - your oral intake has generally been poor because you haven’t felt well. No associated wheeze or stridor.
Time – Cough isn’t worse at any particular time of day. Initially, you were bringing up tiny amounts of green sputum but recently it has been more like teaspoons.
Exacerbating/relieving factors - Paracetamol helped with the fever, but nothing has helped the cough or feeling faint. You have no allergies to anything that you’re aware of and nothing like washing liquid etc. in the house has been changed recently.
Severity – you haven’t been able to go to work and can barely get around the house since a couple of days ago.
Past Medical History
Previous similar episodes - NilOther medical conditions - Nil. No history of asthma.
Previous surgeries - Appendicectomy at age 11. If asked there were no complications.
Drug History
Prescribed - On final day of 5 day course of oral amoxicillin.Over the counter - Paracetamol, cold and flu medicine.
Allergies - None known.
Family History
Your dad had Tuberculosis that he was succesfully treated for before you were born but nothing else. (If candidate pursues this line of questioning – you have no exposure to TB contacts and no travel to areas of high prevalence.)
Social History
Smoking history - Never smokedAlcohol - 1 or 2 pints of beer on the weekends.
Occupation - Marketing consultant. If asked specifically - No known exposure to asbestos, silica or any dust.
Pets (only if specifically asked) - Used to have a hamster. Never owned any birds.
Home - lives with wife and son. No issues at home.
Mobility - Completely independent with no problems.
ADLs - Between you and your wife you do all of the household chores. You also do a lot of the DIY at home.
Systems Review
General/red flags - Experienced fevers. No weight loss or night sweatsNeuro - Bout of dizziness but no LoC
ENT - No ear pain, throat soreness or trouble swallowing
Cardio - no palpitations, no chest pain
GI - No diarrhoea or vomiting, no change in bowel habits.
GU - no lower urinary tract symptoms. No change in urinary habits.
Ideas / Concerns / Expectation
Ideas - Is it some sort of infection?Concerns - I’m really finding it difficult to catch my breath now, am I dying?
Expectations - could you give me some better antibiotics?
Discussion / Questions
The candidate should try and re-assure you (ie acknowledge and explain they’ll do everything they can to help etc) when you ask if you’re going to die. If they do this adequately move on from this. If they attempt to skip over this, then keep bringing the consultation back to this and get gradually more upset…maybe hyperventilate a bit (but not too much, as much as we love the method acting, don’t pass out!)
Patient Results
Please interpret these results
Name:Tony Rogers
DoB: 08/01/1981
PA Radiograph Chest
Date of Study:
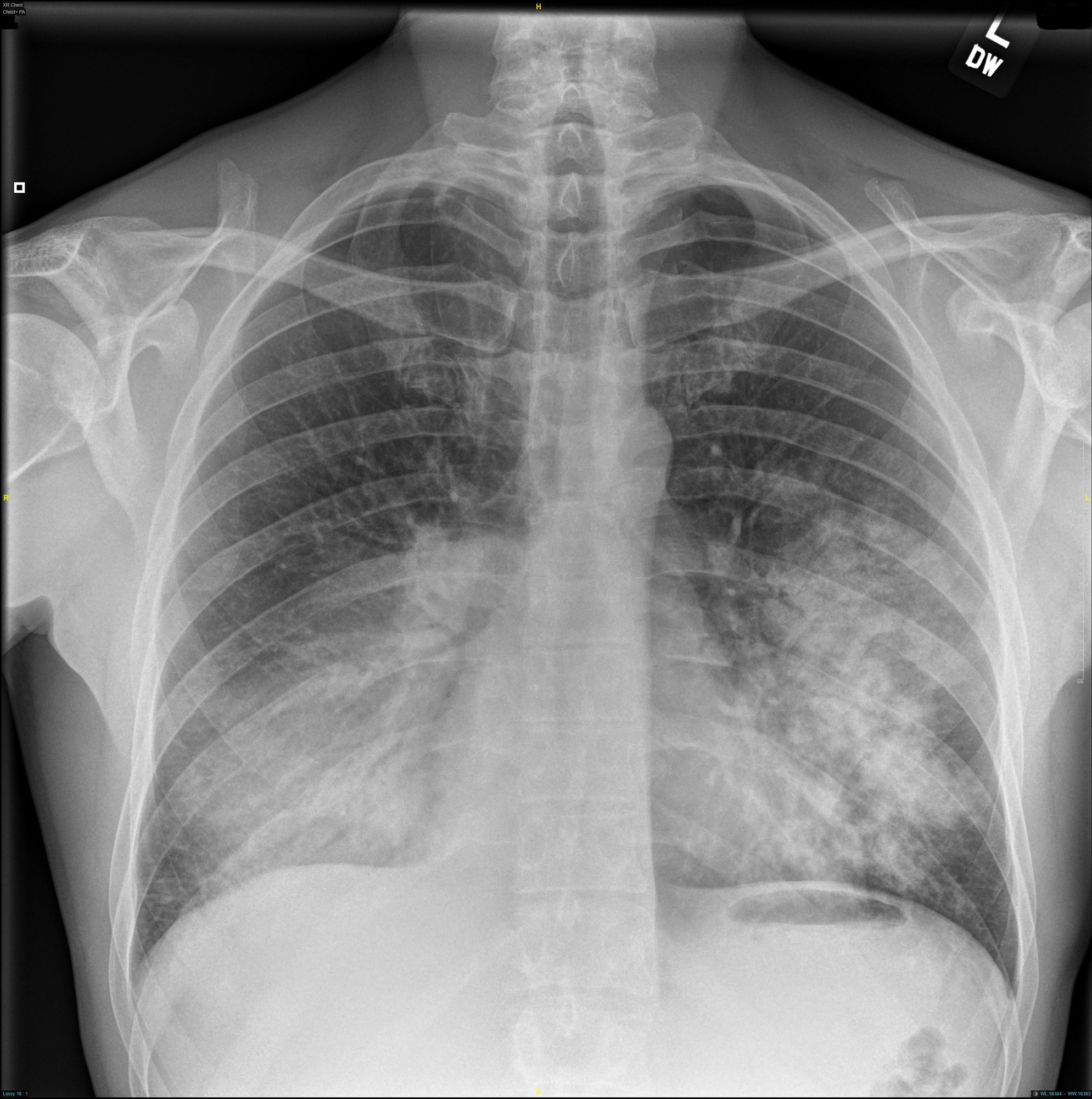
Name:Tony Rogers
DoB: 08/01/1981
ABG taken on 15L via Non-Rebreathe Mask, Resp rate 34, Saturations 88%
Date of Sample:
| Analyte | Value | Normal Range |
|---|---|---|
| pH | 7.29 | (7.35-7.45) |
| PaO2 | 6.3 kPa | (11-13 kPa) |
| PaCO2 | 3 | (4.7-6.0 kPa) |
| HCO3 | 15 | (22-26) |
| Base Excess | -4 | (-2 - 2) |
| Lactate | 6.8 | (0-2) |
| Anion Gap | 19 | (4-12 mmol/L) |
Start the Timer and Begin
Intro
Presenting complaint
Past Medical History
Drug History
Family History
Social History
Systems Reviews
Ideas, Concerns, Expectations
Examiner Instruction
At this point please direct the candidate to move on to investigation requests, diagnosis, and management.
Diagnosis & Interpretation
Please interpret these results
Name:Tony Rogers
Age: 41
PA Radiograph Chest
Date of Study:
ABG results: taken on 15L, Resp rate 34, Saturations 88%
Date of Sample:
| Analyte | Value | Normal Range |
|---|---|---|
| pH | 7.29 | (7.35-7.45) |
| PaO2 | 6.3 kPa | (11-13 kPa) |
| PaCO2 | 3 | (4.7-6.0 kPa) |
| HCO3 | 15 | (22-26) |
| Base Excess | -4 | (-2 - 2) |
| Lactate | 6.8 | (0-2) |
| Anion Gap | 19 | (4-12 mmol/L) |
ABG:
CXR:
Assessment and Management
Submit for Scoring
Tags | Respiratory | Cough | Pneumonia | CAP
Station Written by: Dr Rishil Patel
Peer Reviewed by: Dr Jo Mantio
Want to suggest an edit?
Comment below and we'll get right to it!