Gen Med Examination 5
Station 5
Can’t stop the cough 💨
Candidate Instructions
Setting:
You are a doctor working in General Practice. This 55 year-old patient has presented with increased shortness of breath on exertion and a dry cough for the past 4 months.
Name: James Valentine
Tasks:
1. Please perform a respiratory examination.
2. Summarise your examination findings to the examiner.
3. Request your initial investigations from the examiner.
4. Interpret the provided investigations and give a diagnosis to the examiner.
Simulated Patient Instructions
Briefing
Please act as the patient and reveal signs and results only as the candidate performs actions or requests tests.
Diagnosis: Idiopathic Pulmonary Fibrosis
You are James Scott (age: 56)
You have presented to your GP surgery with progressive shortness of breath on exertion and a dry cough for the past 4 months.
Opening Statement
“My wife convinced me to come in, doc, she says I can’t keep up when we’re walking in the park anymore, and to be fair I do get quite out of puff these days. I think it’s more my cough that’s annoying her but it can’t be anything too serious - I’ve never smoked in my life!”
Appearance and Behaviour
You have been convinced to come today by your wife. She’s noticed that you are becoming more and more breathless on your usual weekend walks and are having to stop for breaks much more often. Plus you just won’t stop coughing! You are convinced it’s just a mixture of age and a tickly cough.
Start the Timer and Begin
Intro
End of Bed Inspection
Peripheral Examination
Clinical Finding -
please show this imagine
to the candidate
as they
examine the hands
Desherinka, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons.
Resp Exam: Look
Resp Exam: Feel
Resp Exam: Listen
Peripheral exam continued
To Complete the Exam
Summary
An Example of a good summary:
Situation: “Today I examined James, a 55 year old man with progressive dyspnoea and dry cough for 4 months.”
Background: “I have no history from the patient at this time.”
Assessment: “Peripheral examination revealed finger clubbing and tachypnea at a rate of 24. Despite this oxygen sats were stable at >96% and there was no central or peripheral cyanosis. There was no peripheral stigmata of fluid overload.
Central exam revealed reduced chest expansion. On auscultation, I heard fine mid- to late-inspiratory crackles in both bases and midzones. There was also increased vocal resonance. The chest was resonant to percussion.”
Recommendation: “To complete my exam I would take a history, and request the following investigations...” (see below for marks on investigations)
Investigation
Examiner Instruction
At this point please direct the candidate to interpret the results below
Please interpret these results:
Name: James Valentine
Age: 56
Date of Results:
| Parameter | Value (L) | Predicted (%) |
|---|---|---|
| FEV1 | 2.5 | 71% |
| FVC | 3.0 | 63% |
| FEV1/FVC | 83% | - |
| TLCO | 3.8 | 42% |
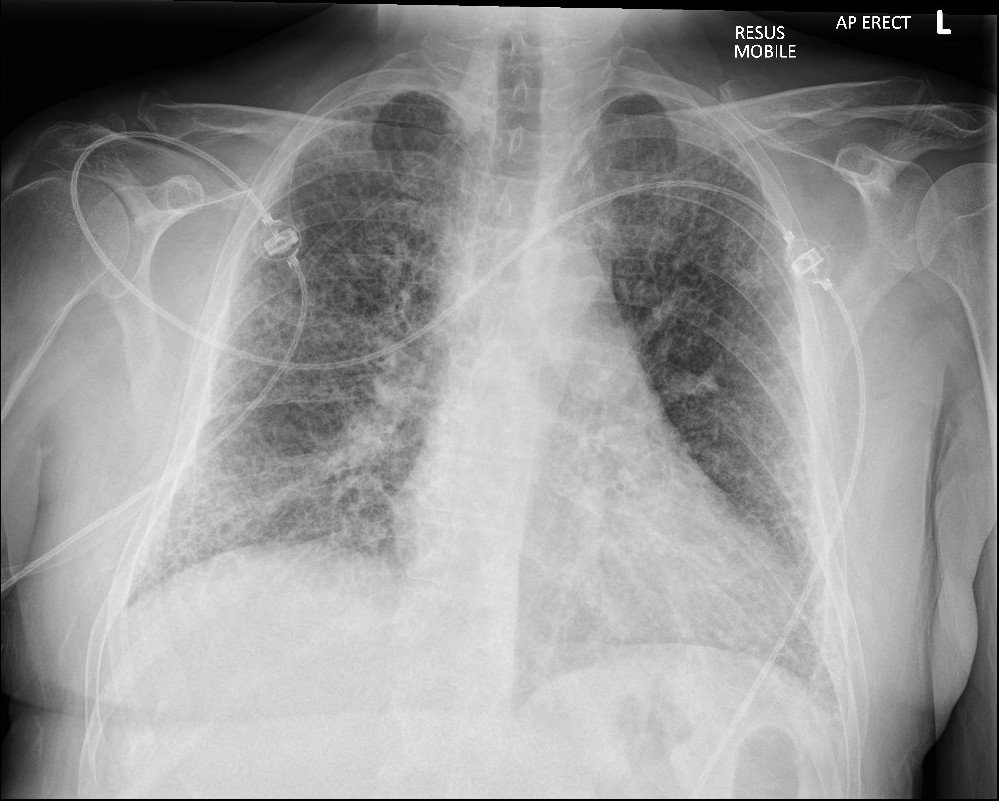
Chest X-Ray
Interpretation & Diagnosis
Submit for Scoring
Summary
James is showing signs of an interstitial lung disease (ILD) - namely in this case idiopathic pulmonary fibrosis but there are several other causes of ILD including:
Environmental / occupational: pneumoconiosis, asbestosis, silicosis, bird fanciers lung.
Iatrogenic: radiotherapy, drugs such as amiodarone and methotrexate
Disease driven: RA, scleroderma, and lupus
Post infective: TB, influenza
Finger clubbing, with exertional dyspnoea, reduced chest expansion (suggestive of restrictive lung disease) and fine “velcro” crackles bilaterally is strongly suggestive of an interstitial lung disease. Idiopathic pulmonary fibrosis tends to present in patients aged 50-70 and is twice as common in men. It is characteristic in IPF for crackles and changes to begin in the lower lobes but they can progress to involve the whole lung parenchyma in advanced disease. As the disease progresses additional signs such as cyanosis, hypoxia, and signs of pulmonary hypertension and right heart failure may appear.
His chest x-ray shows bilateral diffuse fine interstitial markings that are consistent with fibrosis and his pulmonary function tests show a restrictive defect with reduced gas transfer. If you want to impress the examiners always say you would compare the provided XRs with previous images.
To confirm diagnosis, James should be referred to his local Interstitial Lung Disease service where he will be assessed by a respiratory physician and further imaging such as High Resolution CT Chest may be requested. NICE recommends that the diagnosis of IPF is only made with the consensus of a multidisciplinary team based on clinical features, lung function, radiological features, and sometimes pathology. This is due to the diverse and complex nature of Interstitial Lung Disease where there is often overlap with other conditions.
Idiopathic pulmonary fibrosis is the commonest interstitial lung disease and has an average survival from first symptoms of only 3-4yrs. However the disease can run an unpredictable course and most patients with suspected IPF will be followed up indefinitely in the ILD clinic.
Tags | Examination | Respiratory | Breathlessness | CXR | Fibrosis | IPD | Restrictive lung disease | Pulmonary function tests
Station Written by: Dr Jeremie Juan
Peer Reviewed by: Dr Benjamin Armstrong
Want to suggest an edit?
Comment below and we'll get right to it!